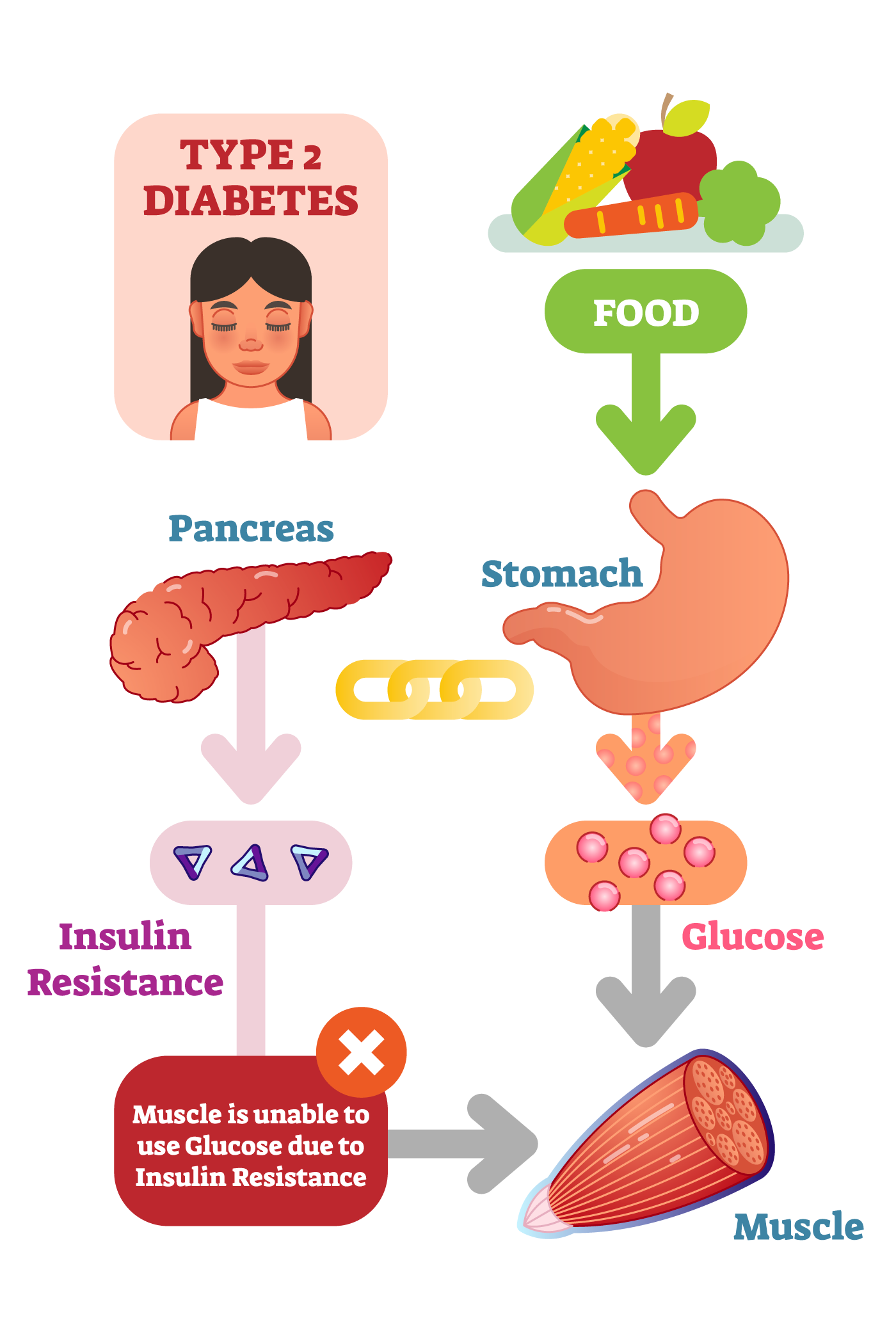
2. What happens with type 2 diabetes?
Type 2 diabetes develops over a period of time. During this time insulin resistance starts, this is where the insulin is increasingly ineffective at managing the blood glucose levels. As a result of this insulin resistance, the pancreas responds by producing greater and greater amounts of insulin, to try and achieve some degree of management of the blood glucose levels.
As insulin overproduction occurs over a very long period of time, the insulin-producing cells in the pancreas wear themselves out, so that by the time someone is diagnosed with type 2 diabetes, they have lost 50 – 70% of their insulin-producing cells. This means type 2 diabetes is a combination of ineffective insulin and not enough insulin. Lifestyle changes may be able to slow this process in some people.
Initially, type 2 diabetes can often be managed with healthy eating and regular physical activity. Over time many people with type 2 diabetes will also need tablets, and/or non-insulin injectable medications and many eventually require insulin injections. It is important to note that this is normal, and taking tablets, non-insulin injectable medications or insulin as soon as they are required can result in fewer long-term complications.
3. What causes type 2 diabetes?
Diabetes runs in the family. If you have a family member with diabetes, you have a genetic disposition to the condition.
While people may have a genetic disposition towards type 2 diabetes, the risk is greatly increased if people have a number of modifiable lifestyle factors including high blood pressure, being overweight, not being active enough, eating a poor diet and having the classic ‘apple shape’ body where extra weight is carried around the waist.
People are at a higher risk of type 2 diabetes if they:
- Have a family history of diabetes
- Are older (over 55 years of age) – the risk increases as we age
- Are over 45 years of age and are overweight
- Are over 45 years of age and have high blood pressure
- Are over 35 years of age and are from an Aboriginal or Torres Strait Islander background
- Are over 35 years of age and are from Pacific Island, Indian subcontinent or Chinese cultural background
- Are a woman who has given birth to a child over 4.5 kgs (9 lbs), or had gestational diabetes when pregnant, or has a condition known as Polycystic Ovarian Syndrome (PCOS)
- Have a mother who had gestational diabetes when they were in utero
4. Symptoms
Many people with type 2 diabetes have no symptoms. As type 2 diabetes is commonly (but not always) diagnosed at a later age, sometimes signs are dismissed as a part of ‘getting older’. In some cases, by the time type 2 diabetes is diagnosed, the long-term complications of diabetes may already be present.